Postpolio syndrome
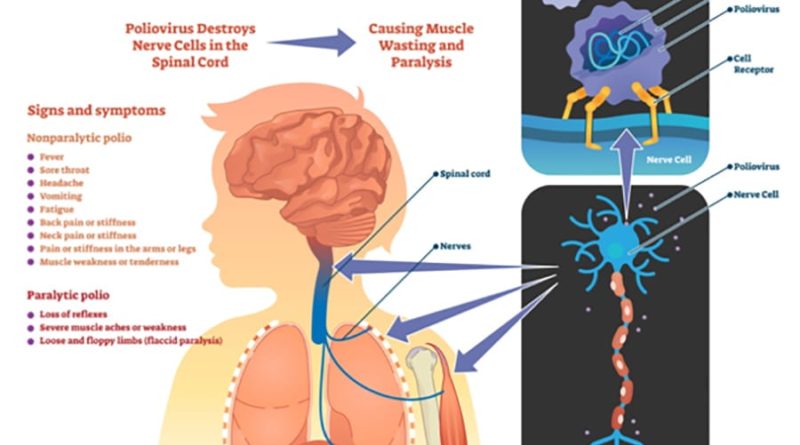
The polio is a neurological disease caused by the polio virus.
Fortunately, thanks to the systematic vaccination campaigns launched in 1963 in our country, it has been virtually eradicated since the late 1960’s. In 1988 the last case was described. In recent years we have been able to find new cases among the immigrant population or after traveling to countries where it is still endemic. It is estimated that in Spain about 35,000 people suffered the consequences of the disease.
Over the years, people suffering from polio may develop locomotor disorders resulting from neurological diseases, such as scoliosis, tendon disorders in the back, or peripheral nerve entrapments by using help. walking or using wheelchairs; respiratory failure, osteoporosis fractures, and ultimately loss of functionality and autonomy.
A small percentage of these people may develop the so-called post-polio syndrome, which is the onset of muscle weakness added to the previous one, without being attributed to disuse. This muscle weakness may or may not be accompanied by fatigue, myalgia, muscle atrophy and the subsequent loss of functionality. If electromyographic changes are observed, we can see that this is truly a post-polio syndrome (Halstead criteria).
In this pathology, the prevention of functional deterioration, through the follow-up by a skilled clinical professional, together with the indicated surgical procedures and a good maintenance rehabilitation are, for now, the best therapeutic option.
Treatment of Postpolio syndrome:
Management includes focusing on preventing or minimizing deformities and maximizing the child’s capability at home and in the community. A child is best treated with an interdisciplinary team that may include the following healthcare providers:
nurse coordinator
neurosurgeon – a surgeon who specializes in operating on the brain and spinal cord.
neurologist – a physician who specializes in conditions of the brain, spinal cord, and nerves.
physical & occupational therapist
orthopaedic surgeon – a surgeon who specializes in conditions of the muscles, ligaments, tendons, and bones.
orthotist – an individual who specializes in making braces and splints.
Specific treatment will be determined by you’re the pediatric team based on:
your child’s age, overall health, and medical history
the extent of the disease
the type of CP
your child’s tolerance for specific medications, procedures, or therapies
expectations for the course of the disease
your opinion or preference
Management of CP includes non-surgical and surgical options. Non-surgical interventions may include:
rehabilitation
positioning aids (used to help the child sit, lie, or stand)
braces and splints (used to prevent deformity and to provide support or protection)
medications (used to help control seizures or to decrease spasticity in the muscles; the medications may be given by mouth or as an injection)
Surgical interventions may include:
orthopedic surgery for, hip dislocations, ankle and foot deformities, and contracted muscles
neurosurgery to remove spasticity including Botox injection, selective dorsal rhizotomy and intrachecal balcaofen pumps.