Spinal cord Rehabilitation
 Spinal cord injuries typically require rehabilitation team members from various specialties who should work together to get you the best possible result. This team will include a physiotherapist, an occupational therapist, a nurse to manage medications and any wounds, a clinical psychologist to assist with the trauma, a dietitian and a doctor who will oversee all the medical care.
Spinal cord injuries typically require rehabilitation team members from various specialties who should work together to get you the best possible result. This team will include a physiotherapist, an occupational therapist, a nurse to manage medications and any wounds, a clinical psychologist to assist with the trauma, a dietitian and a doctor who will oversee all the medical care.
During the various stages of rehabilitation, therapists will focus on maintenance and strengthening of muscle function, redeveloping fine motor skills, and learning adaptive techniques to accomplish your ADLs (Activities of daily life). Along the recovery journey, you and your family members should be educated on the effects of a spinal cord injury and how to prevent complications, and you should be given advice on rebuilding your life and increasing your quality of life and independence.
The duration of rehabilitation and recovery vary depending entirely on the severity of the injury and also how fast a patient start intensive rehabilitation services post injury. The longer one waits, the bigger the risk of permanent disability or debility sinking in.
Choosing Spinal Cord Rehabilitation Program:
Often, life after a major medical event can be quite challenging. The needs and priorities of everyday lives could change to such an extent that we feel like being in a totally new avatar. At this stage, beyond the quick-fix solutions on internet, one will need specialized care to resume to normal lifestyles. Spinal Cord Injuries (SCI) is perhaps one of the most serious orthopedic injuries that require extremely good care and recuperation support. In order to prevent secondary complications, maximize physical functioning and reintegration into community, a structured rehabilitation programme is recommended to those who sustain Spinal cord injuries (SCIs).
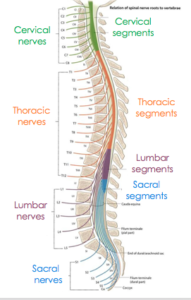
Rehabilitation programmes for spinal cord injuries can be of several types. These are mostly offered in hospitals, standalone clinics and homecare services. The levels of care provided by each of them could be varied and different from one another. Choosing the one that is suited for your condition might be tricky. Spinal Cord Injuries can be either complete or incomplete in nature. Complete injuries lead to permanent loss of the ability of spinal cord to send messages to the brain. At the same time, incomplete injuries leave only partial damage to the spinal cord and some motor and sensory functions remain. Rehabilitation for both these types of injuries is distinct from one another. Based on a patient’s medical history and the extent of damage, the ideal rehabilitation programme for effective recovery is recommended.
Assistive devices
Assistive devices such as wheelchairs have a substantial effect on the quality of life of the patient, and careful selection is important.
Teaching the patient how to transfer from different positions, such as from a wheelchair into bed, is an important part of therapy, and devices such as sliding transfer boards and grab bars can assist in these tasks. Individuals who are able to transfer independently from their wheelchair to the driver’s seat using a sliding transfer board may be able to return to driving in an adapted vehicle. Complete independence with driving also requires the ability to load and unload one’s wheelchair from the vehicle. In addition to acquiring skills such as wheelchair transfers, individuals with a spinal cord injury can greatly benefit from exercise reconditioning. In the majority of cases, spinal cord injury leaves the lower limbs either entirely paralyzed, or with insufficient strength, endurance, or motor control to support safe and effective physical training. Therefore, most exercise training employs the use of arm crank ergometry, wheelchair ergometry, and swimming.
Physical therapists can improve the quality of life of individuals with spinal cord injury by developing exercise programs that are tailored to meet individual patient needs. Adapted physical activity equipment can also be used to allow for sport participation.
Gait training
Body weight supported treadmill training is another intervention that physiotherapists may assist with. Body weight supported treadmill training has been researched in an attempt to prevent bone loss in the lower extremities in individuals with spinal cord injury. Research has shown that early weight-bearing after acute spinal cord injury by standing or treadmill walking (5 times weekly for 25 weeks) resulted in no loss or only moderate loss in trabecular bone compared with immobilized subjects who lost 7-9% of trabecular bone at the tibia. Gait training with body weight support, among patients with incomplete spinal cord injuries, has also recently been shown to be more effective than conventional physiotherapy for improving the spatial-temporal and kinematic gait parameters.
A combination of Body weight supported treadmill training (BWSTT) and robotic-assisted BWSTT is being implemented into some training programs. The benefits include: (1) assist in reproducing leg movements and optimizing gait pattern (speed, step length, amplitude); (2) training sessions can be prolonged and walking speed can be adjusted, increasing motor outcome; (3) provides consistency of movement, where manual interventions/cues by a trainer may be variable (although a trainer should analyze the gait pattern and outcome measures of the training and supervise training).
We may recommend any of the following methods:
Steroid injection
- Trigger point injections
- Epidural steroid injections
- Transforaminal injections
Repetitive transcranial magnatic stimulation (rTMS)
Spinal cord stimulation
Intrathecal baclofen pump